Posture, etiology of a syndromePaolo
Platania
|
Posturology
guidelines and
interdisciplinary case study |
||||||
|
|
|
|
Posturology
|
The case study
|
The backstage
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Pathomechanics
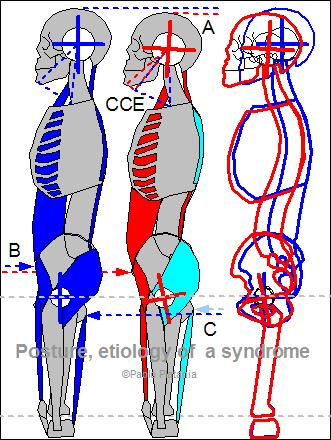
The mechanics section highlights Head forwarding postural strategy (HFPS) concurrent with Mandible Retruding Postural Strategy (MRPS), both featuring Cranio-Cervical Extension (CCE) but with independent features, thus a double pathomechanics and a consequently double diagnostic process is required:- Tongue motor insufficiency (TMI) as first primary pathomechanics for the whole Head Forwarding Postural Strategy (HFPS) + Mandible Retruding Postural Strategy (MRPS) unbalance;
- Dental Conflict (DC) as second primary pathomechanics for the Mandible Retruding Postural Strategy (MRPS) unbalance only;
| Whole body Cranio-Cervical Extension (CCE) muscle spasm | |
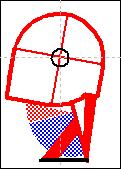
Legend: The model displays the implementation of the Whole body Cranio-Cervical Extension (CCE) muscle spasm and the shape assumed by the scheletal structure under the effect of the pathologic chronic and asymmetric torques: Image 1) Body physiologic posture Image 2) Implementation of Cranio-Cervical Extension (CCE) by Head Forwarding Postural Strategy (HFPS):
Image 3) Physiologic/CCE comparative model REMARK: Although the anatomical displacement induced by Cranio-Cervical Extension (CCE) at first glance may appear symmetric, it is induced by unilateral torque as the pathologic hypertonic muscles are on one side only (Head Forwarding Postural Strategy (HFPS)), this muscle unbalance introduces higly harmful asymmetric torques increasing joint torsion and degeneration. |
 click to enlarge |
 |
After understanding the Whole body implementation of CCE, to better understand the importance (image on the left) of this apparently unmotivated muscle spasm, the local Cranio-Cervical relationship is below isolated and specifically concerned. |
| Physiologic head position (PHP) model | Cervical spine forward inclination model | Cervical spine forward inclination + Atloanto-Occipital Joint (AOJ) extension = Cranio-Cervical Extension (CCE) model |
 |
 |
 |
 click to enlarge |
 click to enlarge |
 click to enlarge |
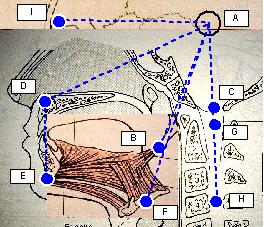
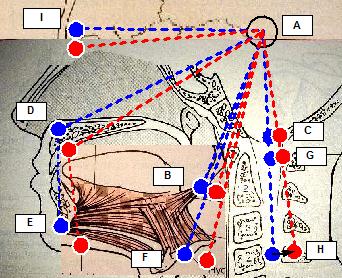
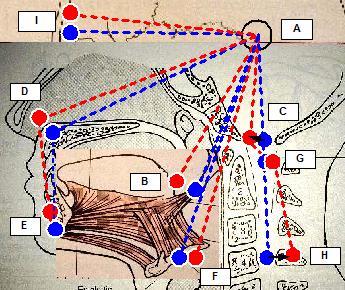
| Legend: Blu: physiologic head position, Red: Cranio-Cervical Extension (CCE), Black: Cranio-Cervical Extension (CCE) motions, Spots: head position markers, dashed lines: cephalometric segments, markers: A (cranial center of rotation), B (styloid process centre of force), C (occipital spinal chord axis), D (maxillary marker), E (chin marker), F (hyoid centre of force), G (atlas spinal cord axis), H (4th vertebra spinal cord axis), I (ocular bulb). |
||
| Physiologic Head Position (PHP) model: positional references marked in blue. | Cervical spine forward inclination model: cranial displacement (red markers) resulting from cervical spine forward inclination which is here represented as fourth vertebra backward motion (HH black arrow) instead of cranial forward motion. | Cranio-Cervical Extension (CCE) model: cranial displacement (red
markers) resulting from the complex adaptation induced by Cranio-Cervical Extension (CCE) [6]:
|
Functional impact: every postural adaptation takes place to promote functionality whenever it becomes undeliverable by physiologic motor control, every compensation induces homeostasis modification and compromises other functional districts, understanding what's improved and what's worsen helps understanding the goal a postural adaptation:
- Sight: under eyes point of view, Cranio-Cervical Extension (CCE) restores a sight angle (AI) that is upward inclined [6] (see also vagal reset), confirming that sight is not a priority to Cranio-Cervical Extension (CCE);
- Mastication: under occlusion point of view, whether the subject is mandible retruded or protruded or normocclusive, Cranio-Cervical Extension (CCE) doesn't seem to promote mastication, suggesting that mastication is not a priority to Cranio-Cervical Extension (CCE);
- Respiration: under tongue point of view, Cranio-Cervical Extension (CCE) features pharynx wall backward motion, mandible forward motion, styloid process up-forward motion and hyoid backward motion, in other words, upper airway patency improvement, as such, prospecting respiration as possible Cranio-Cervical Extension (CCE) priority;
| PATHOMECHANICS: Tongue Motor Insufficiency (TMI) (first primary) | |||||
|
The term Tongue Motor Insufficiency (TMI) scientifically describes unilateral tongue weakness. Head Forwarding Postural Strategy (HFPS) has previously been claimed to be the actuator of unilateral Cranio-Cervical Extension (CCE) which is hereby suspected to compensate highly disabling functional limitations introduced by Tongue Motor Insufficiency (TMI), hence identifying in Tongue Motor Insufficiency (TMI) the first primary pathology. Universally agreed tongue muscular functionality are airway patency, swallowing, phonation and mastication, whereas, although less agreed, head flexion and maxillary arch expansion are considered primary tongue functions as well. Airway patency, head flexion and maxillary arch expansion are pointed to be Head Forwarding Postural Strategy (HFPS) primary pathomechanics, following, the elements supporting it (Ptd01, Ptd02, Ptd03) and the element excluding the alternatives (Ptd04, Ptd05). |
|||||
| # | Description | ||||
| Ptd01 | Upper airway patency mechanics Cranio-Cervical Extension (CCE) induced by this mechanics is defined Active Unilateral Cranio-Cervical Extension (CCE) (AUCCE):
AUCCE mechanics
Extrinsic tongue muscles (genioglossus (GG), hyoglossus (HG) and styloglossus (SG)) are responsible for pharyngeal airway patency [1, 2, 3, 4, 6, 8] as their co-contraction optimises tongue shape and position to reduce airflow resistance, this goal is achieved by rhythmic co-contractions [3, 4] reflex, synchronized with the respiratory muscles, and triggered by the same chemo receptors eliciting the respiratory reflex. Tongue Motor Insufficiency (TMI) induces weak tongue muscle contraction, thus, poor pharyngeal airway patency [18]; this increased airflow resistance may be further enhanced by:
Cranio-Cervical Extension (CCE) role in upper airway patency improvement (as to say airflow resistance reduction) is widely known [16] and accepted (employed even in first aid procedures), hence, is not by chance that human physiology has developed air resistance vagal receptors which are there to elicit a permanent pharyngeal reflex to improve airway patency as soon as an airflow resistance is detected, engaging Head Forwarding Postural Strategy (HFPS) to implement Cranio-Cervical Extension (CCE). This hypothesis highlights an Upper Airway Patency Maintenance Reflex (UAPMR) elicited by unilateral upper airway patency loss owed to Tongue Motor Insufficiency (TMI) and triggering itself the AUCCE spasm featured in Head Forwarding Postural Strategy (HFPS) fully justifying Head Forwarding Postural Strategy (HFPS) presence in the prone and supine positions, moreover, the contralateral physiologic tongue contraction is suspected to further limit airflow by moving the tongue according to the following model: Tongue dislocation model
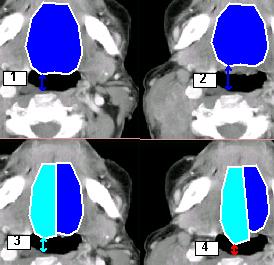
Legend: Tongue dislocation model: the model describes the suspected increased airflow resistance due to increased oxygen demand, the background MRI image is a general (not patient's image) cranial section just above the mandibular arch:
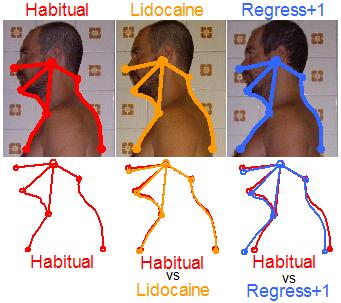
With Tongue Motor Insufficiency (TMI), a unilateral tongue contraction, is neither able to provide the required airway patency with basal respiration (3 vs 1) nor in case of augmented airflow demand (4 vs 2), moreover, unilateral extrinsic muscles contraction induces tongue displacement decreasing the distance between tongue and posterior pharynx wall (red arrow), thus, further stimulating air resistance pharyngeal receptors of the vagus nerve, enforcing the afferent signals inducing a stronger Upper Airway Patency Maintenance Reflex (UAPMR), augmenting AUCCE and worsening Head Forwarding Postural Strategy (HFPS). Please note that extrinsic tongue muscles not only provide tongue intraoral volume regulation (Genioglossus) and vertical elevation (Styloglossus and Hyoglossus), but also cuncur in giving shape to pharynx as Styloglossus lies behind pharynx mucosa and superior pharyngeal constrictor muscle, as such, unilateral tongue weakness may either increase emitongue volume, displace tongue within pharynx and give asymmetric shape to oro-pharyinx, resulting in pharyngeal airflow irregular and asymmetric resistance. Upper Airway Patency Maintenance Reflex (UAPMR) is implemented by a firing pattern that mimics other well known vagal ejective reflexes: the cough reflex and the gag reflex. It is not by chance that these reflexes share the same base firing pattern, given Cranio-Cervical Extension (CCE) is the key condition to provide upper airway patency to maximise either ejection and intake. Since Upper Airway Patency Maintenance Reflex (UAPMR) goal is not to maximize emergency peak ejection but to maximise regular intake, it is implemented as a light Cranio-Cervical Extension (CCE) chronic spasm instead of an abrupt acute Cranio-Cervical Extension (CCE) spasm with ejective feature. Evidence of the existence of Upper Airway Patency Maintenance Reflex (UAPMR) and of its complex firing pattern is provided by the postural reaction of a Head Forwarding Postural Strategy (HFPS) patient to pharyngeal vagal receptors reset done by pharyngeal local appliance of lidocaine 2%, as shown below. Pharyngeal vagal receptors reset
Pharyngeal vagal receptor reset procedure has already been successfully employed [21, 22, 23] in demonstrating the relationship between upper airway receptors and airflow resistance but has never concerned any motor reaction (eg. postural) other than upper airway dimension variation, whereas, the author hereby indeed does. It is author's opinion that airflow resistance increase after vagal receptor reset, occurs as main consequence of the subsidence of the Cranio-Cervical Extension (CCE) spasm in ongoing Head Forwarding Postural Strategy (HFPS) subject, as such, it should NOT occur (or should be much lighter) in healthy posture subjects who fully entrust airway patency maintenance to tongue physiologic rhythmic respiratory contractions [3, 4]. Although apparently denying literature conclusions, the author's claim is not contradictable by existing studies as none of them has been carried out with adequate protocol: "healthy" control subjects have not been sampled according to Head Forwarding Postural Strategy (HFPS) features. According to the undeniably high incidence of Head Forwarding Postural Strategy (HFPS) clues in the population and Head Forwarding Postural Strategy (HFPS) hereby claimed relationship with upper airway patency (TMI), healthy control subjects, without explicit specification, are likely to be HFPS ongoing subjects, as such, the result of these studies on healthy posture subjects is unpredictable and requires further research to be described. Bibliographic support is provided by cross-correlation analysis of the following interdisciplinary literature:
The above findings are relatable by the hypothesis of Upper Airway Patency Maintenance Reflex (UAPMR) triggering Head Forwarding Postural Strategy (HFPS) to implement AUCCE in response to increased airflow resistance introduced by Tongue Motor Insufficiency (TMI) (hence, preventing snoring during non REM sleep), confirming the consequences of Head Forwarding Postural Strategy (HFPS) loss on airflow (snoring when Cranio-Cervical Extension (CCE) muscular tone drops during REM sleep). Further supporting evidences:
Airflow asymmetric afferences localization
Legend:
All these findings allow to state that GG, HG and SG actively participate in respiration and a that Tongue Motor Insufficiency (TMI) might result in respiration insufficiency and consequent permanent Upper Airway Patency Maintenance Reflex (UAPMR) to induce unilateral muscular spasm (Head Forwarding Postural Strategy (HFPS)). |
||||
| Ptd02 | Head flexion mechanics
PUCCE mechanics Tongue muscles pulling on the styloid process and on the mandible (behind chin) feature a cranial flexion moment arm and, given the continuous and strong tonic contraction for pharyngeal airways patency [8], exert direct hyoid-cranial flexion force. These literature overlooked features is hardly escaped to physiology which may rely on GG, HG, SG, stylohyoid (SH) and infrahyoid muscular chain for AOJ flexion, undeniable healthy posture indicator. The following models provide explanation of the theory. |
||||
| Physiologic Head Posture (PHP) model | Physiologic Head Posture (PHP) vs Cranio-Cervical Extension (CCE) model |
||||
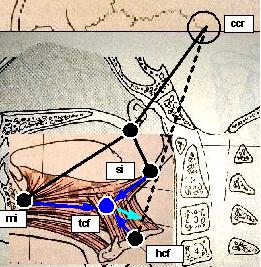 click to enlarge |
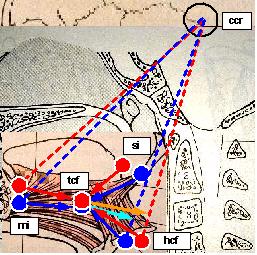 click to enlarge |
||||
|
Legend: Blu: PHP, Red: Cranio-Cervical Extension (CCE), Black: Fixed relationship, Cian: PHP cranial flexion moment arm, Orange: Cranio-Cervical Extension (CCE) cranial flexion moment arm, Spots: head position markers, dashed lines: cephalometric segments, solid arrows: muscular forces and resultant vectors (color), bony forces (black), markers: ccr (cranial centre of rotation), si (styloid insertion), mi (mandible insertion), hcf (hyoid centre of force), tcf (tongue centre of force). Conventions:
|
|||||
|
Physiologic Head Position (PHP) model demonstrates the Atlanto Occipital Joint (AOJ) flexing moment arm (Cian arrow) exerted by co-contraction of extrinsic tongue muscles during tongue activity, moreover it highlights the fact that whatever tongue muscle contraction induces a cranial flexion, the model assumes the following:
|
Physiologic Head Posture (PHP) vs
displays a good attitude
of the tongue to induce AOJ flexion in the PHP (Cian arrow)
whereas, with increasing Cranio-Cervical Extension (CCE), GG-HG-SG force (tcf)
produces a growing cranial flexion moment arm (orange arrow) to facilitate tongue muscles
restoring the AOJ angle, thus, in case of Tongue Motor Insufficiency (TMI), Atlanto Occipital Joint (AOJ)
extension may not be corrected by GG-HG-SG and has to be compensated by
forward inclination of the cervical spine generating Cranio-Cervical Extension (CCE) hence Head Forwarding Postural Strategy (HFPS).Cranio-Cervical Extension (CCE) model |
||||
|
Mandible depressors are also capable of Atlanto Occipital Joint (AOJ) flexion, the action is provided by geniohyoid (GH), digastric (DG), stylohyoid (SH) and Milohyoid (MH) complex, the model is not presented as it's out of the scope of the present analysis.
Although AUCCE plays the key role in Head Forwarding Postural Strategy (HFPS), PUCCE seems to be reasonably involved as impairment in tongue muscles may introduce cranial flexion weakness, but, without proper measurements, it is not possible to quantify the extent of Cranio-Cervical Extension (CCE) induced by PUCCE. Moreover, Head Forwarding Postural Strategy (HFPS) is present regardless from head position, whereas PUCCE is only triggered head upright, as such, PUCCE may not be responsible for provoking Cranio-Cervical Extension (CCE) in the prone and supine position. These findings allow to state that GG, HG and SG actively participate in cranial inclination tuning and that a Tongue Motor Insufficiency (TMI) might result in cranial displacement (PUCCE) |
|||||
| Ptd03 | Maxillary arch expansion mechanics Tongue muscles pressure against palate is reasonably suspected [11, 13] to have a plastic function over the maxillary alveolar process and maxillary teeth axis orientation. The daily amount (about 2000 x 3 kg) of swallowing induced force pulses [11] and continuous tongue elevation pressure [8] (to hold the tongue high against the nasopharynx during nose breathing) is transferred to the palate and teeth and counterbalances cheeks and lips opposite forces, hence, being SG equipped with enviable palatal lateral expansion moment arm and being GG able to frontally expand the arch, tongue muscles are suspected to have a primary role in expansion. Based on the patient's finding examination (Ecl19, Ecl20, Ecl22, Ese08, Eot05), a relationship between Tongue Motor Insufficiency (TMI) and maxillary insufficiency seems more then suspect, the next step is to determine which is primary on which other:
Maxillary arch insufficiency is an irreversible structural under development (at least not spontaneously reversible within acceptable times) of the maxillary arch and, given its etiopathogenetic role in Mandible Retruding Postural Strategy (MRPS), is considered a second primary pathomechanics and requires a dedicate diagnostic/therapeutic process but only after first primary process is successfully terminated. Refer to section maxillary arch insufficiency for thorough mechanics exploration. These findings allow to state that GG, HG and SG actively participate in maxillary arch expansion and that a Tongue Motor Insufficiency (TMI) may result in maxillary arch insufficiency, hereby theorized to be primary over Mandible Retruding Postural Strategy (MRPS). |
||||
| Ptd04 | Why Tongue Motor Insufficiency
(TMI) may not be secondary ? Tongue Motor Insufficiency (TMI) is supposed not to be secondary to other function unbalance for the following reasons:
|
||||
| Ptd05 | Why doesn't swallowing, phonation and
mastication mechanics affect Mandible
Retruding Postural Strategy (MRPS) and Head
Forwarding Postural Strategy (HFPS) ? Despite some clinical literature proposes these functions to be involved in posture, their pathomechanics is still controverse. Although the disorder of these functions is part of platania's syndrome and is secondary to Tongue Motor Insufficiency (TMI), it is NOT considered to be primary to Head Forwarding Postural Strategy (HFPS) and Mandible Retruding Postural Strategy (MRPS) for the following reasons:
|
||||
| PATHOMECHANICS: Dental Conflict (DC) (second primary) | ||
|
Mandible
Retruding Postural Strategy (MRPS) is been supposed to be the
actuator of bilateral Cranio-Cervical Extension (CCE), the reasonable relationship
between Dental Conflict (DC) and
TMJ disorder (mandible retrusion) lead to speculate that Dental Conflict (DC) is the second primary pathomechanics. Following, the elements supporting this hypothesis (Pdc01) and the element excluding the alternatives (Pdc02). |
||
| # | Description | |
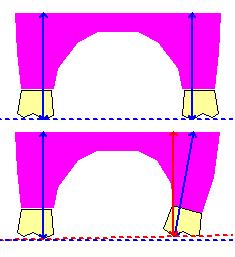
| Pdc01 | Dental Conflict (DC) mechanics Cranio-Cervical Extension (CCE) induced by this mechanics is defined Structural Bilateral Cranio-Cervical Extension (CCE) (SBCCE):
SBCCE mechanics Dental Conflict (DC) mechanics over TMJ disorder eliciting condition is as follows: neurological afferences (trigeminal nerve) produced by pathologic teeth contacts generate inhibitory reflexes directed to the responsible muscles aimed to avoiding every type of harmful motion, these reflexes successfully grant teeth safety but on the other side generate pathologic torques on mandible provoking the TMJ disorder. TMJ disorders are widely suspected to induce, among several other symptoms, postural unbalances. Although Mandible Retruding Postural Strategy (MRPS) seems reasonably related to TMJ disorder, the pathomechanics of its impairing capabilities over posture is unclear. Although several symptoms are ascribable to TMJ disorder (condile dislocation, mastication disorder and temporal muscles painful contractures), postural disorder doesn't appear to be mediated by these conditions, the author in spite proposes the following hypothesis to justify Cranio-Cervical relationship modification (CCE) consequent to TMJ disorder:
Physiologic maxillary and mandibular arches get together (centric occlusion) when molar and pre molar teeth on one arch contact the opposite molar and pre molar teeth on the opposite arch in normocclusion TMJ position. Normocclusion TMJ is not functional to the patient's bite as it would cause upper and lower incisors to contact (due to upper incisors crowding, Ecl19) preventing molar and pre molar contact. Molar occlusion, in context of incisor teeth crowding, is achievable with mandible retrusion. |
|
| Pdc02 | Why not other TMJ displacements at Mandible Retruding Postural Strategy (MRPS) origin ? Mandible retrusion is not the only TMJ displacement, nevertheless is considered the main responsible for Mandible Retruding Postural Strategy (MRPS) for the following reasons:
|
|
Lack of vertical dimension |
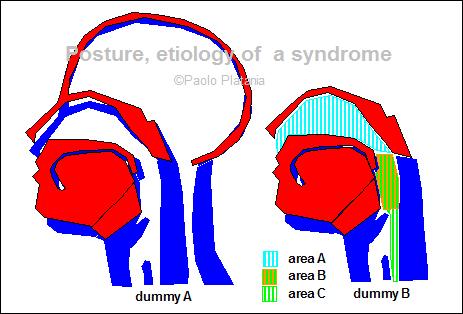
Facial muscles symmetry |
|
 click to enlarge |  click to enlarge |
|
|
Bugs report and technical issues notification to the webmaster are highly apreciated
|
| Posture, etiology of a syndrome - ©2008 Paolo Platania |